Clinical Case Scenario
A 26‑year‑old woman, five months post–renal transplant for autosomal dominant polycystic kidney disease, was admitted to the ICU with hematemesis, fever, and altered sensorium. On arrival, she was hypotensive (BP 84/65 mmHg) with severe anemia (Hb 5 g/dL).
After initial resuscitation and elective intubation for airway protection, she underwent CT angiography, which revealed multiple aneurysms in the coeliac and mesenteric arterial tree with active bleeding from the gastroduodenal artery (GDA). She underwent successful embolization of the GDA and was transferred back to the ICU for post‑procedural care.
She was empirically started on piperacillin–tazobactam and vancomycin. Blood cultures grew Enterococcus faecium, prompting escalation to meropenem, voriconazole, and trimethoprim–sulfamethoxazole for broader coverage. Given her recent transplant, the nephrology team advised continuation of immunosuppressants. All routine medications were continued except aspirin (withheld due to bleeding risk). Her whole blood tacrolimus trough level was subtherapeutic (5 ng/mL), so the dose was increased from 4 mg/day to 6 mg/day.
Her condition stabilized, and she was extubated on day 6.
On day 8, she developed a headache and severe hypertension (BP 180/100 mmHg). Neurological examination showed no focal deficits except for tremors. Later that evening, she developed visual disturbances and progressive coma.
Laboratory Findings
What is the most appropriate next step in the definitive management of this patient.

Author’s Name:
Trishita Saha
Field of Specialization: Anesthesiology, Critical Care Medicine, ECMO
Qualifications / credentials: MBBS, MD, DM Critical Care Medicine, FIECMO(Fellowship in ECMO)
Current Designation: Associate Consultant
Department: Respiratory Medicine and ECMO unit
Institute: Apollo Multispeciality Hospitals, Kolkata
Email ID:trishitasaha2006@gmail.com

Author’s Name:
Khalid Zafar
Field of Specialization: Critical Care Medicine
Qualifications / credentials: MBBS, MD, DM Critical Care Medicine (SGPGI)
Current Designation: Assistant Professor (ad hoc)
Department: Critical Care Medicine
Department: Critical Care Medicine
Institute: Sanjay Gandhi Postgraduate Institute of Medical Sciences, Lucknow
Email ID: drkhalidzafar@icloud.com

Author’s Name:
Swapna Chitra Vijayakumaran
Field of Specialization: Anaesthesiology, Critical Care Medicine
Qualifications / credentials: MBBS, MD, DM (TMH, Mumbai)
Current Designation: Fellow Intensive Care
Department: Intensive care medicine
Institute:
The Canberra Hospital , ACT, Australia
Email ID: drswapnacharie1990@gmail.com

Author’s Name:
Mohd Saif Khan
Field of Specialization: Anaesthesiology, Critical Care Medicine
Qualifications / credentials: MBBS, MD, DNB, Postdoctoral fellowship (Critical care) DM (Critical Care Medicine), MNAMS
Current Designation: Consultant & Program Director, Adult Critical Care
Department: Critical Care Medicine
Institute: King Hamad University Hospital, Bahrain
Email ID: mohd.saif@khuh.org.bh, drsaif2k2@gmail.com


A 70-year-old man with known decompensated alcoholic liver cirrhosis presents to the ICU.
History
Vital Signs
Laboratory Findings
Which of the following is the most appropriate way to use 3% NaCl during CRRT to safely manage this patient’s hypernatremia?
The same patient is started on continuous renal replacement therapy (CRRT). On day 1, his laboratory results are:
To buffer sodium loss, you decide to infuse 3% NaCl via a central line during CRRT.
(Assume distribution volume of Na = 0.6 × body weight, and [Na] in 3% NaCl = 513 mmol/L).
What is the approximate rate (mL/hr) of 3% NaCl infusion required to limit the serum sodium drop to less than 10 mmol/L/day?
Clinical Case Scenario
A 56-year-old man with a 5-year history of HIV-1, previously managed with elvitegravir, emtricitabine, and tenofovir disoproxil fumarate (TDF) but lost to follow-up, presented to the ICU with acute hypoxic respiratory failure. He reported a week of fever, dry cough, and musculoskeletal pain, treated with NSAIDs. In the emergency department, he was hypertensive (200/111 mmHg), tachypneic (RR 26), and hypoxic, requiring 15 L/min oxygen via non-rebreather mask to maintain SpO2 >94%. Examination revealed bilateral pitting pedal edema to the knees, oliguria, and volume overload. He was stabilized and admitted to the ICU.
Labs: Creatinine 4.7 mg/dL (baseline 2.5 mg/dL), RBC 3-5/HPF, glucosuria (+), proteinuria (3+), spot urine protein/creatinine ratio 5.2 mg/mg (ref <0.10 mg/mgCr), albumin 2 g/dL, total protein 6.5 g/dL, CPK 200, Ultrasound KUB: enlarged kidneys with increased echogenicity, pH 7.29, Na 148, K 3.1, CD4/CD8 ratio 0.11, CD4 cells 86/μL, HIV viral load 119,000 copies/mL.
A renal biopsy, performed due to rapidly declining renal function and nephrotic-range proteinuria, revealed collapsing focal segmental glomerulosclerosis (FSGS), marked interstitial inflammation, dilated cystic tubules, and tubular epithelial inclusion bodies.
Continuous renal replacement therapy (CRRT) was initiated, and NSAIDs were discontinued.
What is the most appropriate next step in the management of this patient?
Clinical Scenario
A 68-year-old male with poorly controlled type 2 diabetes and peripheral vascular disease is admitted to the ICU following emergency debridement of a necrotizing soft tissue infection involving his left lower limb. He presents with septic shock: hypotension requiring norepinephrine, high-grade fever, and altered mental status. Blood cultures grow Staphylococcus aureus, and broad-spectrum antibiotics including vancomycin are initiated.
Over the next 24 hours, the patient develops oliguric acute kidney injury, classified as KDIGO Stage III, with rising creatinine and fluid overload which eventually lead to requirement of invasive mechanical ventilation. Renal replacement therapy is initiated using Coupled Plasma Filtration Adsorption (CPFA) to address both renal dysfunction and the overwhelming inflammatory response (see Figure 1).

Figure 1. Coupled Plasma Filtration Adsorption (courtesy: https://mozarcmedical.com)
Despite standard vancomycin dosing (15 mg/kg IV q12h), his trough levels remain persistently subtherapeutic at 7 µg/mL (target: 15–20 µg/mL). Repeat cultures remain positive, and clinical signs of infection persist.
Which of the following mechanisms most likely explains this finding?
Clinical Case Scenario
A 45-year-old man working as a ground cleaner for an international airline presents to the emergency department with altered mental status and oliguria. He has a history of chronic alcohol use and was found unconscious near a maintenance area with multiple empty containers of aircraft de-icing fluid. Laboratory investigations reveal a serum creatinine of 3.5 mg/dL, a high anion gap metabolic acidosis, and calcium oxalate crystals in the urine

figure 1. De-icing procedure of aircraft

Figure 2. De-icing fluid to remove ice from aircraft body
Question: What is the most appropriate initial treatment?
Clinical Case Scenario
A 58-year-old female presents to the Emergency Department with a several-day history of progressive, debilitating fatigue and generalized malaise. She reports new-onset dark, tea-colored urine (cola-colored) and a significant reduction in her urine output. She also notes new headaches and visual disturbances, which she attributes to feeling unwell. Her home medications include:
Vital Signs at Presentation:
Physical Examination Findings:
Key Laboratory Findings:
Test | Result | Reference / Baseline |
Hemoglobin (Hb) | 8.7 g/dL | (Down from 12 g/dL 2 weeks prior) |
Platelets | 85,000/µL | (Thrombocytopenia) |
Lactate Dehydrogenase (LDH) | 580 U/L | (Markedly elevated) |
Haptoglobin | < 30 mg/dL | (Undetectable) |
Peripheral Smear | 2+ schistocytes | (Evidence of microangiopathic hemolysis) |
Serum Creatinine | 3.2 mg/dL | (Baseline: 1.1 mg/dL) |
Urinalysis | ||
Appearance | Dark/Amber | |
Blood | 3+ | |
Protein | 2+ | |
Microscopy | 20-30 RBCs/HPF (microscopic hematuria) | No casts seen |
C4d Staining (recent biopsy) | Negative | |
Donor-Specific Antibodies (DSA) | None Detected |
|
What is the MOST likely diagnosis?
Clinical Case Scenario
A 65-year-old patient is 3 weeks post-double lung transplantation. He presents with a rapid rise in serum creatinine (from baseline 0.9 mg/dL to 2.8 mg/dL over 5 days). Urine output remains adequate. His immunosuppression regimen includes tacrolimus (trough level 18 ng/mL), mycophenolate mofetil, and prednisone. In view of decline in post transplant pulmonary function test values, the patient underwent a CT angiogram of thorax. He has also developed a new onset dry cough with lethargy and irritability.
On examination he is conscious, alert. Vital parameters as:
HR: 84/min
BP:128/76 mmHg
RR: 16/min
Temp: 37 C
Chest X-ray shows no acute pathology.
Lactate: 1.4 mmoL/L
Urinalysis shows:
Protein +
Sugar Absent
Ketone Absent
Nitrite Absent
Pus cells 1-2
RBCs Nil
Casts Nil
Crystals Nil
Epithelial cells Absent
What is the MOST likely cause of his acute kidney injury?
Clinical Case Scenario
A 16-year-old girl is anaesthetized for scoliosis surgery. After induction of anaesthesia, the patient, who is under anaesthesia with isoflurane and nitrous oxide, suddenly develops unexplained tachycardia, a high end-tidal CO2 (EtCO2) of 54 mmHg, and a fever of 39°C.
The anaesthesia team administers an initial bolus of dantrolene sodium at 1 mg/kg. Despite this treatment, the patient’s tachycardia and elevated EtCO2 levels do not improve. She is then transferred to the intensive care unit (ICU).
What is the most appropriate next step in the management of this patient while in the ICU?
Clinical Case Scenario
A 68-year-old male is admitted to the intensive care unit with septic shock due to severe community-acquired pneumonia and hypoxemic respiratory failure. He is hemodynamically stabilized on norepinephrine at 0.15 mcg/kg/min and has received an initial 30 mL/kg of crystalloid fluids, followed by an additional 3 liters of crystalloid over the next 24 hours, guided by pulse pressure variation monitoring. After 24 hours, the following data is available:
Based on above information, tick one best response from each question:
Question 1a. What is the most appropriate interpretation of this patient’s renal profile?
Question 1b: What is the most appropriate interpretation regarding the need for renal replacement therapy (RRT) in this patient?
Clinical Care Scenario
A 62-year-old woman with type 2 diabetes (on metformin 1g twice daily), chronic hypertension (on Lisinopril 100 mg BD), and peripheral arterial disease presents to the emergency department with a 2-day history of severe watery diarrhoea, nausea, and vomiting. She had been caring for her grandson, who recently had gastroenteritis. On arrival, she is confused and hypotensive (BP 70/39 mmHg). Laboratory findings reveal:
She is diagnosed with severe lactic acidosis. Despite discontinuation of metformin and Lisinopril, aggressive fluid resuscitation, and vasopressor support, she develops pulseless electrical activity (PEA) cardiac arrest. After successful resuscitation, continuous renal replacement therapy (CRRT) is initiated in ICU. Blood culture is growing E. coli O157:H7.
What is the most likely primary cause of this patient’s life-threatening lactic acidosis?
Clinical Case Scenario
An elderly woman presents to the emergency room with generalized weakness, headache, and confusion. Her blood pressure is 220/105 mmHg. Physical examination reveals skin thickening of the extremities, facial telangiectasias, and decreased oral aperture. Laboratory studies reveal creatinine levels of 3.5 mg/dL, hemoglobin at 7.0 g/dL, a platelet count of 75,000/mm³, and lactate dehydrogenase at 700 U/L.
What is the appropriate initial treatment?
Clinical Case Scenario
Mr. James Thornton, a 68-year-old male with a significant medical history of uncontrolled hypertension, diabetes, and chronic kidney disease on maintenance hemodialysis, presents to the emergency department with a 3-day history of productive cough, fever, and progressive dyspnea. On initial evaluation, he is febrile, tachypneic, and hypotensive with a mean arterial pressure (MAP) of 55 mmHg and a heart rate of 110/min. He has also become oliguric for the last 8 hours and continues to be hypotensive even after receiving a fluid bolus and norepinephrine infusion. Bedside point-of-care ultrasound was performed where the Doppler profile of the LVOT demonstrated a dagger-shaped appearance (Figure 1).
What is the most appropriate next step?

Figure 1. Continuous wave doppler across LVOT (Picture courtesy-Geske JB et al.Clin Cardiol 2009;32:397)
Clinical Case Scenario
A 36-year-old female presented with history of 1 day of fever associated with rash, and breathlessness, rapidly progressing to severe metabolic acidosis, refractory septic shock requiring multiple vasopressors, acute kidney injury, and disseminated intravascular coagulopathy with multi-organ dysfunction. Physical examination revealed multiple petechial patches (Figure 2) all over the body. Despite aggressive management, including intubation, mechanical ventilation, broad-spectrum antibiotics, and fluid resuscitation, the patient’s condition deteriorates, ultimately leading to cardiac arrest and death within 36 hours of ICU admission.
A POCUS of the abdomen of this patient during resuscitation revealed the findings which are shown in figure 1. A screening echo was normal with good left ventricular systolic function. Preliminary blood culture findings show gram-negative diplococci.
Which of the following conditions best describes the rapidly progressive shock and widespread purpuric rash?

Figure 1: POCUS scan of right adrenal gland
(Case courtesy of Mohammad walid Ahmad Amin, Radiopaedia.org, rID: 192003)

Figure 2: Petechial patches on body
(Image sourced from DermNet)
Clinical Case Scenario
A 37-year-old woman with a history of type 2 diabetes mellitus arrived at the emergency department with a history of five days of worsening severe left upper quadrant abdominal pain that radiated to her left flank. She also reported fever, chills, nausea, vomiting, and general malaise. Upon arrival, her vital signs were a heart rate of 110 bpm and a axillary temperature of 39 °C. Physical examination revealed tenderness in her left costovertebral area, but her abdomen was not tender. Lab tests confirmed a urinary tract infection with a white blood cell count of 12,510 cells/mm3 and an increase in immature white blood cells. Additionally, the serum creatinine level of 5.71 mg/dL prompted the physician to perform a bedside Point-of-Care Ultrasound (POCUS) of the left kidney (figure 1) to check for urinary tract obstruction.

Figure 1: POCUS of the left kidney
(Case courtesy of Maulik S Patel, Radiopaedia.org, rID: 17283)
Which of the following POCUS findings would be most characteristic and concerning for acute emphysematous pyelonephritis?
Clinical Case Scenario
A 70-year-old man, known hypertensive managed on telmisartan and thiazide diuretic was brought to the hospital by her family due to confusion and lethargy. For the last week, he had been complaining of low oral intake. He seemed disoriented during inspection, but his hemodynamics were stable. His symptoms started around two days ago and the plasma sodium level was found to be 120 mmol/L. He experienced convulsions at the emergency room after an hour of arriving at ER and was given 3% saline to treat it. Within the following 12 hours, his blood sodium level quickly returned to 136 mmol/L. His neurological condition then worsened. An urgent MRI brain showed the following image as shown in figure 1.

Figure 1: T2 weighted imaging showing hyperintensities in basis pontis (white arrow)
(Case courtesy of Frank Gaillard, Radiopaedia.org, rID: 2598)
Which of the following best describes the pathophysiological process causing the patient’s neurological decline?
Clinical Case Secnario
A 37-year-old male with a long-standing history of chronic smoking (15 pack-years) presented to the emergency department with the acute onset of excruciating, constant, epigastric pain that radiated sharply to his back. This severe pain began approximately 12 hours before presentation and was accompanied by multiple episodes of non-bloody, bilious vomiting and complete loss of appetite (anorexia). He is a chronic smoker (15 pack years) who denies any history of alcohol abuse, recent abdominal trauma, prior surgeries, or known history of gallstones. There has been no history of recent medication intake. Upon admission, he was diagnosed with moderate acute pancreatitis secondary to severe hypertriglyceridemia (serum triglyceride 2902 mg/dL), as supported by initial lab findings and imaging (modified CT scan severity index of 6/10) (Figure 1). He also exhibited signs of systemic inflammatory response syndrome (SIRS), including a fever of 38.5°C on arrival and a respiratory rate of 30 breaths/minute.
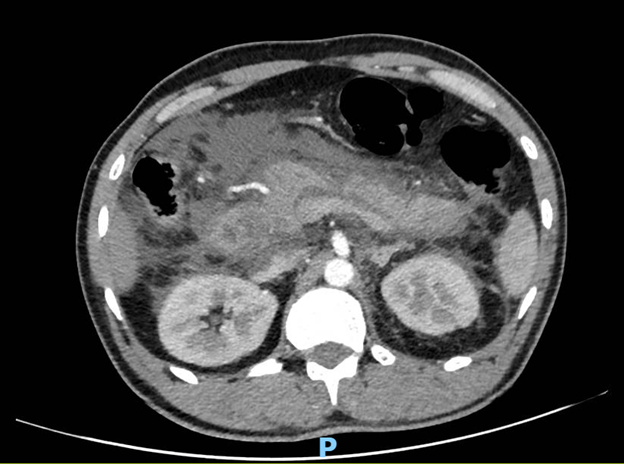
Figure 1: Contrast-enhanced CT abdomen
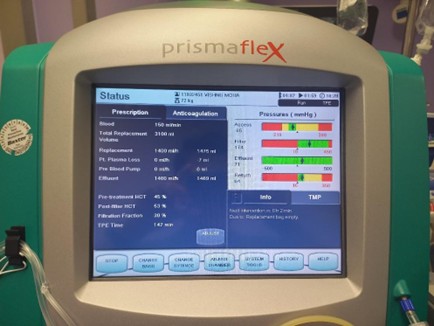
Figure 2: Settings of the extracorporeal therapy

Figure 3: Machine used for extracorporeal therapy
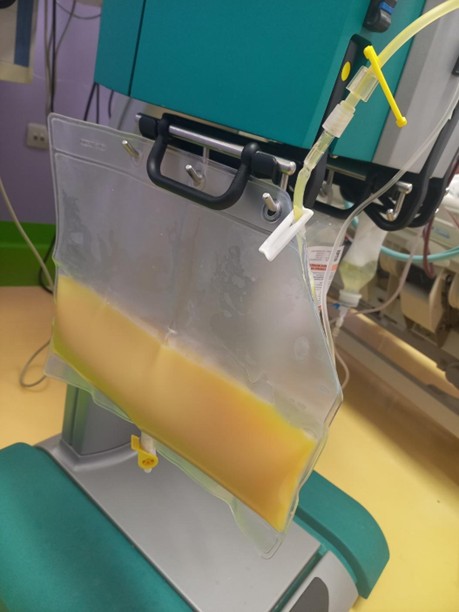
Figure 4: Filtered plasma of the patient, collected as effluent in the bag (yellowish colored as the effluent is lipemic secondary to the high level of triglycerides)
Given the patient’s presentation and the ongoing management, which of the following statements regarding the role of the extracorporeal therapy being used (Figures 2, 3, and 4) in hypertriglyceridemia-induced acute pancreatitis is most accurate?
Clinical Case Scenario
A 59-year-old man who has a history of renal transplant 3 years ago on immunosuppression suddenly developed respiratory distress, he was diagnosed with COVID-19 ARDS with a PaO2/FiO2 ratio of less than 70 for the past one day.VV-ECMO was initiated for the ARDS, he developed AKI one day post-cannulation, and his Hb was 7 g/dl. The parameters on ECMO machine and his chest X-ray are shown below:

What is the next best course of management?
Clinical Case Scenario
A 68-year-old male presents to the ED with acute onset of severe dyspnoea, pleuritic chest pain, and lightheadedness. He has a history of recent prolonged immobility.
Upon arrival, he is hypotensive (BP, 70/40 mmHg), tachycardic (HR, 130 bpm), tachypneic (RR, 38 bpm), and profoundly hypoxemic (SpO2, 78% on room air), requiring immediate tracheal intubation. Physical exam reveals a swollen, tender right lower extremity.
Initial labs show a significantly elevated D-dimer and a platelet count of 65,000/µL. A lower limb Doppler reveals a deep venous thrombosis (DVT) in the bilateral proximal femoral veins. An immediate CT pulmonary angiogram (CTPA) reveals a large saddle pulmonary embolus (PE) with significant right ventricular strain.
Which of the following is the most appropriate management option at this time point?
Clinical Case Scenario
A 45-year-old man with abdominal sepsis caused by duodenal perforation was transferred to the ICU from the operating theatre in view of septic shock (on norepinephrine 0.2 microgram/kg/minute) and acute kidney injury. He requires emergent dialysis in the ICU. A 12 French triple-lumen dialysis catheter is uneventfully placed via the right internal jugular vein by a senior registrar in the ICU. Post-insertion, a chest X-ray (CXR) shows the catheter tip in the mid-right atrium (RA).
What is the most urgent next step for this patient?
Clinical Case Scenario
A 56-year-old female has a recent history of undergoing a heart transplant. She is admitted to the intensive care unit with new-onset oliguria. Her baseline serum creatinine prior to her heart transplant was 0.8 mg/dL. She had a stable post-transplant serum creatinine at 1.2 mg/dL on her maintenance immunosuppression regimen of cyclosporine and mycophenolate mofetil. However, over the past 48 hours, her serum creatinine has increased to 2.8 mg/dL, and her urine output has decreased to less than 20 mL/hour. Her BUN/serum creatinine ratio is noted to be 10. She is hemodynamically stable, and a renal ultrasound shows no evidence of obstruction. Her most recent cyclosporine trough level was 200 ng/mL.
Which of the following is the MOST likely cause of this patient’s acute kidney injury?
Clinical Case Scenario
A 16-year-old male with a history of type 1 diabetes mellitus presented in the emergency department. His condition has worsened over the past 3 days. He reported extreme thirst and has been drinking large quantities of fluids and juice. His urine output was very high during this period, and on history taking, it was found out that he had not been compliant with his insulin regimen for the last month. His urine flow rate is measured at 12 mL/min in the emergency room using a uroflowmeter.



Despite excreting large quantities of glucose in the urine, her plasma glucose concentration remains unchanged over the observation period.
What is the primary mechanism responsible for this patient’s polyuria?
Clinical Case Scenario
A 68-year-old male with a long-standing history of chronic kidney disease secondary to poorly controlled hypertension and type 2 diabetes mellitus has been managed conservatively with dietary restrictions and medications for the past five years. His estimated glomerular filtration rate (eGFR) has been progressively declining. Over the last six months, he has developed worsening symptoms of uremia, including fatigue, nausea, loss of appetite, and pruritus. His most recent laboratory results, obtained two days ago, showed a blood urea nitrogen (BUN) of 110 mg/dL and a creatinine level of 8.5 mg/dL. He has not yet received renal replacement therapy. Today, he presents to the emergency department complaining of new-onset, sharp, retrosternal chest pain that is exacerbated by lying flat and relieved somewhat by sitting forward. He also reports increasing shortness of breath and light-headedness. His wife mentions that he seems more tired and less responsive than usual.
On physical examination, he appears pale and diaphoretic. His vital signs are as follows:
Blood Pressure: 90/60 mmHg
Heart Rate: 115 beats per minute
Respiratory Rate: 28 breaths per minute, laboured
Oxygen Saturation: 90% on room air
Auscultation of his chest reveals distant heart sounds and a soft pericardial friction rub. His jugular veins are markedly distended even when sitting upright. Peripheral pulses are weak and thready. There is no evidence of peripheral oedema on this examination.
Repeat laboratory tests show worsening azotemia with a BUN of 125 mg/dL and creatinine of 9.1 mg/dL, along with elevated potassium and phosphate levels.
The following is the echocardiography image of the patient done as a routine NephroPOCUS scan

Which of the following accurately describes a method for quantitatively evaluating this patient’s cardiac condition using echocardiography?
Clinical Case Scenario
A 60-year-old woman presents to the emergency department with persistent vomiting for 5 days. She has a history of hypertension, dyslipidaemia, chronic knee osteoarthritis, and pyloric stenosis due to long-term NSAID use. In the ED, she develops hypotension (BP 80/54 mmHg) and tachycardia (HR 115 bpm). On bedside POCUS assessment, her IVC diameter is 0.5 cm, which is collapsing to 30%. Lab results show:
Na⁺: 132 mmol/L
K⁺ : 2.8 mmol/L
Cl⁻ : 82 mmol/L
HCO₃⁻ : 38 mmol/L
pH: 7.52
Lactate: 4 mmol/L
Urea: 20 mmoL/L
Creatinine: 155 micromol/L (Baseline creatinine 95 micromol/L)
The ICU team advises aggressive resuscitation with 0.9% normal saline. After four litres of fluid administration along with 40 mmol of IV potassium chloride, BP improves to 102/64 mmHg, and follow-up labs are as follows:
Na⁺ : 135
K⁺ : 3.1 mmol/L
Cl⁻ : 97 mmol/L
HCO₃⁻ : 33 mmol/L
pH: 7.47
Lactate : 2.5 mmoL/L
Which one of the following is the correct statement regarding fluid resuscitation in this patient?
Clinical Case Scenario
A 62-year-old male with a history of hypertension and dyslipidaemia presents to the emergency department with severe retrosternal chest pain, sweating, and shortness of breath. A 12-lead ECG shows ST-segment elevation myocardial infarction (STEMI). The patient rapidly deteriorates, developing profound hypotension and signs of cardiogenic shock. The patient is intubated and he is started on inotrope infusion, and the patient is transferred to the ICU.
In ICU, shock persists despite escalating doses of inotropes. Veno-arterial extracorporeal membrane oxygenation (VA-ECMO) is initiated via the femoral artery and femoral vein. Gradually an improvement in haemodynamics is observed.
Over the next few hours, the ICU team notes that the patient’s lower extremities remain warm and well-perfused, with good pulse oximetry readings. However, the upper extremities and face appear cyanotic. Arterial blood gas (ABG) analysis reveals a significant discrepancy: blood from the right radial artery (upper body) shows ‘PaO₂ 45 mmHg,’ while blood from the femoral arterial line (lower body, ECMO-supported) shows ‘PaO₂ 95 mmHg.’
Over the next 24 hours, the patient develops oliguria (urine output 100 mL in last 24 hours). Laboratory findings include:
– Serum creatinine: 2.4 mg/dL (trends up from 1.0 mg/dL)
– Blood urea nitrogen (BUN): 48 mg/dL (trends up from 11 mg/dL)
– K⁺: 5.8 mEq/L
– pH: 7.18, HCO₃⁻: 14 mEq/L
– Urinalysis: Muddy brown granular casts
Which of the following is the most appropriate next step in management?
Clinical Case Scenario
A 62-year-old diabetic and hypertensive male with chronic kidney disease (CKD) with eGFR) of 50 mL per minute per 1.73 m2 presents with generalized weakness and hyperkalemia. The lab investigations are given below:
Lab values:
pH: 7.31
HCO₃⁻: 17 mEq/L
PaCO₂: 38 mmHg
Na⁺: 138 mEq/L
K⁺: 6.2 mEq/L
Cl⁻: 108 mEq/L
Urine pH: 5.0
Urine Na⁺: 25 mEq/L
Plasma Aldosterone: Low
Which of the following is the most likely cause of this patient’s acid-base disturbance?
Clinical Case Scenario
A 62-year-old male with a history of hypertension and dyslipidemia presents to the emergency department with severe retrosternal chest pain, sweating, and shortness of breath. A 12-lead ECG was performed, suggesting ST-segment elevation Myocardial infarction (STEMI). The patient rapidly deteriorated, developing profound hypotension and signs of cardiogenic shock. The patient’s trachea was intubated and inotrope was started, however, the shock did not reverse and worsened. Due to refractory cardiogenic shock, veno-arterial extracorporeal membrane oxygenation (VA-ECMO) is initiated via the femoral artery and vein. Initial VA-ECMO support provides hemodynamic stability, and the patient is transferred to the intensive care unit (ICU).
Over the next few hours, the ICU team observes that the patient’s lower extremities remain warm and well-perfused, with good oxygen saturation readings from the pulse oximeter. However, the patient’s upper extremities and face exhibit cyanosis. Arterial blood gas analysis reveals a significant discrepancy with blood drawn from the radial artery (representing upper body oxygenation) shows a lower PaO2 whereas blood drawn from the femoral arterial line (representing lower body oxygenation from the ECMO circuit) shows a higher PaO2.
Which of the following statements is true regarding the phenomenon occurring in this patient?
Clinical Case Scenario
A 35-year-old male is brought to the emergency department after being found unconscious in his apartment. His roommate reports that the patient had been complaining of severe muscle pain and dark urine for the past two days, as shown below. His roommate also described the patient having run a marathon the day prior to becoming unconscious. Upon examination, the patient’s legs are swollen and tender. Laboratory results reveal a markedly elevated creatinine kinase (CK) level of 15,000 U/L, elevated creatinine, and myoglobinuria. Although the first line of treatment for this condition is hydration with IV fluids, which of the following statements is true?

Clinical Case Scenanio
Jonathan Hayes, a 50-year-old kidney transplant recipient, presented with a gradual decline in graft function one-year post-transplant. His creatinine had risen from 1.72 mg/dL to 3.75 mg/dl with proteinuria, with a urea level of 90 mg/dL, despite unremarkable renal ultrasound findings. He remained on tacrolimus and mycophenolate mofetil, with a tacrolimus trough level of 6.4 ng/mL. Laboratory tests showed an elevated C-Reactive Protein of 28.7 mg/dL, but no obvious source of infection was identified on imaging or urinalysis, and CMV-PCR was negative. The abdominal CT-angiogram showed the following:

What can be the cause of his worsening graft function?
Clinical Case Scenario
A 57-year-old male kidney transplant patient presents with nausea, vomiting, headaches, and lethargy. Five days earlier, he was treated with Paxlovid for a mild SARS-CoV-2 infection. His past medical history includes kidney transplantation managed with prednisone, tacrolimus, and mycophenolate. Examination reveals blood pressure of 176/94 mmHg, serum creatinine of 213 µmol/L (baseline 130 µmol/L), and tacrolimus trough level of 56 µg/L.
What is the most likely cause of his acute kidney injury?
Clinical Case Scenario
A 57-year-old male was admitted with acute hypoxemic respiratory failure due to Influenza A pneumonia with ARDS. After an initial trial of prone ventilation failed, he was placed on veno-venous (V-V) ECMO. Initially, at low ECMO flows of 2 L/min, his pulse oximeter/peripheral oxygen saturation improved. However, as the flow was gradually increased to 4 L/min, his oxygen saturation levels worsened. A review of his chest X-ray (Figure 1) was conducted.

Figure 1: Chest Xray of the patient after cannulation
*Figure adapted from www.intensiveblog.com
Which of the following statements is true regarding the patient’s current condition?
Clinical Case Scenario
An 82-year-old woman with advanced heart failure, chronic kidney disease stage 4 (baseline creatinine 2.8 mg/dL), and metastatic lung cancer with extensive bony metastases is admitted to the ICU with septic shock due to a urinary tract infection. Despite receiving broad-spectrum antibiotics, IV fluids, and norepinephrine for persistent hypotension, she has been anuric for 24 hours, and her creatinine has risen to 5.8 mg/dL. Her trachea is intubated and she is sedated with propofol and remifentanil infusions, her Sequential Organ Failure Assessment (SOFA) score is 16. Her prior medical records indicate that during a previous hospitalization, she expressed a wish to “focus on comfort and avoid unnecessary interventions,” but no formal advance directive or do-not-resuscitate (DNR) order was completed.
Her daughter insists on starting renal replacement therapy (RRT), stating, “We have to do everything possible,” while her son is concerned about prolonging her suffering. The ICU team is divided: one physician suggests a time-limited trial (TLT) of RRT, while another believes it would be futile given her poor prognosis. The patient’s nurse raises concerns about the burdens of aggressive care in this scenario.
Which of the following is the most appropriate next step in managing this complex situation?

 Where, pCO2: partial pressure of carbon dioxide, Na+ : Sodium, K+ : Potassium, Ca++ : Calcium, Mg++ : Magnesium, Cl- : Chloride Gamblegrams, named after physician James L. Gamble, are bar diagrams displaying the relative abundance of extracellular anions and cations and are commonly used to analyze acid-base disorders. Based on the gamblegrams shown below, select the appropriate combination of labels.
Where, pCO2: partial pressure of carbon dioxide, Na+ : Sodium, K+ : Potassium, Ca++ : Calcium, Mg++ : Magnesium, Cl- : Chloride Gamblegrams, named after physician James L. Gamble, are bar diagrams displaying the relative abundance of extracellular anions and cations and are commonly used to analyze acid-base disorders. Based on the gamblegrams shown below, select the appropriate combination of labels.

Clinical Case Scenario
Recent advancements in the management of acute decompensated heart failure (ADHF) have focused on optimizing decongestion strategies through combination diuretic therapy. Clinical trials, such as ADVOR, CLOROTIC, and others, have evaluated novel interventions to enhance diuretic efficacy, overcome resistance, and improve patient outcomes.
Which of the following statements best reflects the evidence from these studies?
Clinical Case Scenario
The initiation of renal replacement therapy (RRT) in critically ill patients remains a topic of debate. The ELAIN, AKIKI, STARRT-AKI, and IDEAL ICU trials sought to identify the best timing for starting this therapy in patients wit acute kidney injury. The results of these studies have provided valuable insights, yet they highlight the complexity of managing acute kidney injury (AKI) in critical care settings.
Select the INCORRECT statement about the four trials mentioned above.
Clinical Case Scenario
Incorporating kinetic GFR (kGFR) into clinical practice offers a promising approach to enhancing the accuracy of kidney function assessment in acute settings.
Which of the following best describes the concept of kGFR?
Clinical Case Scenario
A 38-year-old female, gravida 7, para 3, living 3, abortus 3 (G7P3L3A3) at 28 weeks of gestation with a monochorionic, diamniotic twin pregnancy underwent emergency lower segment caesarean section (LSCS) for pre-eclampsia. She was also a known case of gestational diabetes mellitus (GDM). Although her intra-operative course was uneventful, on POD 4, she developed gradually progressive and persistent abdominal pain, distension, with tenderness on palpation. A new-onset fever was noted with urine output of 250 ml over the past 24 hours. Her lab investigations on POD 4 revealed elevated C-reactive protein (CRP, 180 mg/L), and urine analysis showed leukocytes 50-100 per high-power field and positive leukocyte esterase, suggestive of UTI. Renal function tests revealed a serum creatinine of 3.4 mg/dL and BUN of 133 mg/dL. Contrast-Enhanced CT (CECT) abdomen and pelvis revealed significant free fluid in the peritoneal cavity with evidence of intraperitoneal extravasation of contrast at the dome of the bladder (Figure 1). A pigtail catheter was inserted for ascitic fluid drainage. The normal bladder anatomy is shown in the figure below (Figure 2).

Figure 1: Intraperitoneal extravasation of contrast and a clear defect in the dome of the bladder (black arrow) (Image courtesy: www.radiopaedia.org)

Figure 2: Normal bladder anatomy
Which of the following statements is incorrect regarding this case?
Clinical Case Scenario
A 65-year-old male patient with a history of chronic kidney disease and hypertension was admitted to the ICU with severe metabolic acidosis. Despite standard medical therapy, his peripheral venous blood gas analysis shows pH: 7.23, base excess [BE]: -4 mEq/L, PaCO2: 32 mm Hg, and lactate: 6 mmol/L. The medical team decided to administer sodium bicarbonate to correct the acidosis.
Question: What is one of the main potential risks associated with the use of sodium bicarbonate therapy in ICU patients with severe metabolic acidosis and AKI?
Clinical Case Scenario
A 60-year-old male with a history of hypertension and diabetes mellitus is admitted to the hospital with a three-day history of vomiting, decreased oral intake, and reduced urine output. On initial assessment, he appears lethargic, with dry mucous membranes, poor skin turgor, and cool extremities. His blood pressure is 85/60 mmHg, heart rate is 110 bpm, and respiratory rate is 22 breaths per minute. The patient’s laboratory results reveal elevated serum creatinine (2.8 mg/dL, baseline 1.0 mg/dL), elevated blood urea nitrogen (BUN) of 45 mg/dL, and electrolyte imbalances.
The clinical team is concerned about acute kidney injury (AKI) in the context of hypovolemia and discusses the importance of accurate volume status assessment to guide resuscitation and prevent further kidney damage. Appropriate fluid resuscitation is considered to optimize renal perfusion.
Question: Which of the following methods is most appropriate for assessing intravascular volume status in this patient with AKI?
Clinical Case Scenario
A 45-year-old male undergoing treatment for diffuse large B-cell lymphoma at a day care center develops oliguria 24 hours post-chemotherapy. Despite aggressive hydration, rasburicase, and allopurinol, the patient remains oliguric. Laboratory results reveal a serum potassium of 7.2 mEq/L, serum phosphate of 8.5 mg/dL, serum calcium of 6.0 mg/dL, serum uric acid of 20 mg/dL, and a creatinine level of 4.5 mg/dL. A critical care referral is made after the patient exhibits stridor and generalized muscle cramps. The 12-lead ECG shows a QTc interval of 550 msec.
What is the next best step in management?
Clinical Case Scenario
A 22-year-old male with Burkitt lymphoma arrives at oncology day care with acute abdominal pain, nausea, vomiting, and confusion shortly after starting R-CODOX-M (rituximab, cyclophosphamide, vincristine, doxorubicin, and methotrexate). His vitals are BP 90/67 mmHg, HR 121/min, SpO2 95% on room air, and respiratory rate 25/min. Venous blood gas analysis shows: pH 7.23, PCO2 26 mmoL/L, HCO3 17 mmoL/L, Lactate 2.24 mmoL/L.
Laboratory tests reveal the following:

Despite initial aggressive intravenous fluid resuscitation and treatment with rasburicase, the patient’s urine output has dropped significantly, and he is now anuric.
Which of the following is the most likely complication this patient is experiencing?

“I discovered, that the saline solution which I had used had not been prepared with distilled water, but with pipe water supplied by the New River Water Company. As this water contains minute traces of various inorganic substances, I at once tested the action of saline solution made with distilled water and I found that I did not get the effects described in the paper referred to. It is obvious therefore, that the effects I had obtained are due to some of the inorganic constituents of the pipe water”
These were the words of Sydney Ringer, a British clinician and physiologist, is recognised for formulating the ‘Ringer’s solution,’ which facilitated the maintenance of isolated frog heart contractions, ultimately contributing to the creation of an isotonic solution utilised in medical research.
Which particular inorganic compound referred to here had the most profound impact in maintaining the frog heart contractions?
Clinical Case Scenario
A 45-year-old female is admitted to the Intensive Care Unit (ICU) with confusion, fever, and petechial rash. She has a history of fatigue, easy bruising, and intermittent abdominal pain over the past two weeks. On physical examination, she is febrile (38.5°C), hypotensive (BP: 95/60 mmHg), and tachycardic (HR: 120 bpm). She has scattered petechiae on her extremities and mild scleral icterus. Initial laboratory findings reveal severe thrombocytopenia (platelet count: 12,000/µL), microangiopathic hemolytic anemia (hemoglobin: 7.5 g/dL with schistocytes seen on blood smear), elevated lactate dehydrogenase (LDH), and normal coagulation parameters. Renal function tests show acute kidney injury (creatinine: 3.2 mg/dL), and a urine dipstick is positive for hemoglobin without red blood cells on microscopy.
The clinical presentation and lab findings strongly suggest a diagnosis of thrombotic thrombocytopenic purpura (TTP). The patient is immediately started on plasma exchange therapy along with corticosteroids. Due to significant renal impairment, continuous renal replacement therapy (CRRT) is initiated concurrently to manage fluid overload and electrolyte imbalances. The ICU team discusses the therapeutic goals and complications associated with TTP and the rationale for the chosen interventions.
What is the primary goal of plasma exchange therapy in the management of TTP?
Clinical Case Scenario
A 35-year-old male patient with severe hepatic encephalopathy due to liver failure presents with confusion, lethargy, and asterixis. Laboratory tests show significantly elevated ammonia levels (210 µmol/L) and impaired kidney functions (urea 55 mmol/L and creatinine 210 µmol/L). Lactate and bicarbonate levels in blood gas are at 10 mmol/L and 14 mmol/L respectively. Despite maximal medical therapy, including lactulose and rifaximin, the patient’s condition worsens. Continuous Renal Replacement Therapy (CRRT) is initiated.
What is the primary rationale for using CRRT in this patient, and what key technical considerations should be noted?
Clinical Case Scenario
A 48-year-old man presents with cough and fever, and a nasopharyngeal swab confirms influenza A. He begins treatment with oseltamivir but returns to the ED within 24 hours with high-grade fever, multifocal lung opacities on chest x-ray, and respiratory failure necessitating intubation and ICU admission. Blood cultures and bronchoalveolar lavage (BAL) reveal methicillin-resistant Staphylococcus aureus (MRSA). After receiving a 2-liter crystalloid bolus and appropriate antibiotics, he develops progressive hypotension. A central venous catheter (CVC) is inserted via the right internal jugular vein. His vital signs show mean arterial pressure (MAP) at 45 mm Hg, central venous pressure (CVP) at 11 mm Hg, central venous oxygen saturation (ScVO2) at 89%, arterial lactate at 10.2 mmol/L, and urine output of 10 cc/hr over the last 4 hours.
Which of the following statements is correct about the next step in management?
Clinical Case Scenario
After undergoing a 12-hour liver transplant surgery, a 56-year-old man received 15 units of RBCs, 8 units of FFP, 4 units of platelets, and 500 mL of albumin. He was transferred to the intensive care unit in a stable condition but developed signs of septic shock four hours later. Broad-spectrum antibiotics were initiated.
What is the most likely source of sepsis in this patient?
Clinical Case Scenario 1
A 72-year-old man is hospitalized for respiratory failure caused by pneumonia acquired in the community. Blood cultures confirm pneumococcal infection. He receives appropriate antibiotics but requires intubation due to worsening hypotension despite IV fluids. Norepinephrine and vasopressin are initiated to manage the worsening hypotension. Over the next 72 hours, his creatinine levels elevate from 1.0 to 4.6 mg/dl, and his urine output decreases to 0–5 mL/hr. A family conference is scheduled to discuss the potential need for continuous renal replacement therapy (CRRT).
Which of the following statements is the most accurate?
Clinical Case Scenario 1
A 58-year-old woman with a history of hypertension arrived at the Emergency Department with symptoms including fever, nausea, vomiting, and confusion. Her vital signs were as follows; temperature: 39.3°C, heart rate: 98/min, blood pressure: 132/64 mm Hg, respiratory rate: 26/min, and oxygen saturation (SaO2): 92% on room air. During the physical examination, she exhibited renal angle tenderness. Laboratory tests revealed a white blood cell count of 22,000/mm³, serum creatinine of 2.3 mg/dL (baseline 0.7 mg/dL), and more than 50 white blood cells per high power field on urine microscopy. A non-contrast CT scan of the abdomen and pelvis showed right perinephric stranding without stones or hydronephrosis. Blood and urine cultures were taken, ceftriaxone was administered, and she was admitted to the ICU.
Which of the following statements about this patient’s acute kidney injury (AKI) is most accurate?
Question 2
Which of the following statements regarding acute graft-versus-host disease (GVHD) after renal transplantation is TRUE?
Question 1
Which of the following statements is incorrect regarding the physiological process depicted in the figure?

Clinical Case Scenario 2
A 52-year-old male with septic shock and multiple organ failure is undergoing continuous renal replacement therapy (CRRT) in the ICU. The team decides to use citrate anticoagulation to manage his therapy.
What is the primary advantage of using citrate anticoagulation in CRRT?
Clinical Case Scenario 1
A 54-year-old male (weight 85 kg, height 175 cm) with a medical history of Type 2 diabetes mellitus, essential hypertension, chronic kidney disease (Stage 5), ischaemic heart disease, and heart failure with reduced ejection fraction (HFrEF) was admitted to the ICU with septic shock secondary to pneumonia. Currently he is on broad-spectrum antibiotics, vasopressors, and mechanical ventilation. His hemodynamic parameters and lab investigations are as follows:
Hemodynamics:
Blood Pressure: 90/50 mmHg (on norepinephrine at 0.1 mcg/kg/min)
Heart Rate: 110 bpm
Central Venous Pressure (CVP): 12 mmHg
Cardiac Output: 4 L/min
Urine output of 20 to 25 ml/hr
Labs:
Haemoglobin: 9.5 g/dL
WBC: 15,000 /µL
Platelets: 120,000 /µL
Serum creatinine: 6.5 mg/dL
Blood Urea Nitrogen (BUN): 70 mg/dL
Potassium: 5.8 mEq/L
Arterial Blood Gas (ABG): pH 7.25, PaCO2 30 mmHg, PaO2 75 mmHg, HCO3- 16 mEq/L
He was initiated on intermittent hemodialysis (IHD) for acute kidney injury and severe metabolic acidosis.
Initial settings: Blood flow rate 300 mL/min, Dialysate flow rate 500 mL/min, Ultrafiltration goal 2 litres over 4 hours.
1 hour into dialysis, his blood pressure dropped to 80/45 mmHg, and heart rate 120 bpm. His norepinephrine infusion rate increased to 0.2 mcg/kg/min; 500 mL of normal saline bolus was administered.
A review of the dialysis solution composition shows the following:
Base: bicarbonate 25 mM
Sodium: 130 mM
Potassium: 3.5 mM
Calcium: 1.5 mM (3.0 mEq/L)
Magnesium: 0.375 mM (0.75 mEq/L)
Dextrose: 5.5 mM (100 mg/dL)
Phosphate: none
Dialysis solution temperature: 33°C
At this point, to improve the hemodynamic tolerance of the ongoing intermittent hemodialysis session, the following changes are recommended, except:
Question 1
A 65-year-old, female (Weight: 70 kg, Height: 160 cm), with a previous medical history of end-stage renal disease (ESRD) on hemodialysis, essential hypertension, diabetes mellitus type 2, peripheral vascular disease admitted to the ICU with acute pulmonary oedema secondary to fluid overload. On day one, she presented with shortness of breath, orthopnoea, and bilateral lower extremity oedema.
Her vitals are as follows- Blood Pressure: 170/95 mmHg; Heart Rate: 100 bpm; Respiratory Rate: 28 breaths/min; Oxygen Saturation: 88% on room air, which improved to 95% on 5 L/min nasal cannula.
Her laboratory investigations are:
Hemoglobin: 10.5 g/dL
WBC: 11,000 /µL
Platelets: 140,000 /µL
Serum Creatinine: 8.2 mg/dL
Blood Urea Nitrogen (BUN): 90 mg/dL
Potassium: 6.2 mEq/L
BNP: 1500 pg/mL
Arterial Blood Gas (ABG) values are as follows– pH 7.30, PaCO2 : 50 mmHg, PaO2 : 65 mmHg, HCO3 : 24 mEq/L
A Chest X-ray showed bilateral pulmonary infiltrates consistent with pulmonary edema.
Emergency hemodialysis was planned, and a dialysis catheter insertion was scheduled as the patient does not have a functioning arteriovenous fistula.
Which of the following factors has the greatest impact on the flow rate of a dialysis catheter and which site should be selected (considering all available sites)?
Clinical Case Scenario 2
A 67-year-old woman with chronic heart failure presents with worsening dyspnea and significant peripheral edema. She is diagnosed with cardiorenal syndrome, and her renal function has declined considerably.
Which statement best reflects the management of cardiorenal syndrome (CRS)?
Question 1
A 60-year-old male patient with a history of diabetes mellitus and chronic kidney disease is admitted to the ICU with acute kidney injury (AKI). He also has a recent history of severe diarrhea. His arterial blood gas analysis is as follows:
pH:7.25,
HCO3: 17 mEq/L,
Na: 142 mEq/L
K: 3.3 mmoL/L
Cl: 112 mEq/L
Albumin: 3.0 mg/dL
Random blood sugar: 5 mmoL/L
Lactate: 2.3 mmoL/L
Which of the following is the most likely cause of his metabolic disorder?
Clinical Case Scenario 2
A 45-year-old male presents to the emergency department with confusion and oliguria for one day. He has a history of discoloration of his eyes for the last five days. Laboratory tests reveal:
AST 320 U/L, ALT 410 U/L, GGT 229 U/L, INR > 1.5, Serum creatinine of 300 µmol/L.
Positive ANA (1:320), Positive Smooth Muscle Antibody (1:40), Elevated IgG levels.
Abdominal Ultrasound: Enlarged liver with mild hepatic inflammation, no evidence of cirrhosis or Budd-Chiari syndrome.
Other Tests: Negative viral hepatitis panel, normal ceruloplasmin, elevated ferritin. His GCS deteriorated from 13 to 7, for which the trachea was intubated and the patient was transferred to ICU. Inj Methylprednisolone 125 mg IV OD was started. Despite initial supportive measures, his condition continues to deteriorate.
Which of the following extracorporeal therapies is most appropriate to manage this patient’s condition?
Question 1

Shortly after a new Medical Renal Unit (MRU) opened, this outbreak led to 40 cases soon including deaths among patients and staff. The outbreak prompted the establishment of an advisory group led by Lord Rosenheim, which gave a series of recommendations and crucial containment measures. Despite precautions, the outbreak’s severity, had a lasting impact on infection control practices in medical settings. This outbreak in the 19th century was the subject of Colin Douglas’s popular outrageous novel “The Houseman’s Tale”, and it continues to influence the way physicians think about the risks of infection.
Choose the combination of place, year, causative organism and primary mode of outbreak transmission that is being referred to here.
Clinical Case Scenario 2
A 45-year-old male with severe respiratory distress syndrome is initiated on ECMO. During his stay in the ICU, he develops signs of acute kidney injury (AKI). The medical team is considering the best approach for renal replacement therapy (RRT) due to his hemodynamic instability.
Question: In this patient with AKI on ECMO, which of the following statements is correct?
Clinical Case Scenario 1
A 64-year-old man is admitted to the hospital with a cough, fever, and low oxygen levels. He quickly progresses to respiratory distress, necessitating endotracheal intubation. A chest x-ray reveals widespread bilateral lung opacities. An arterial blood gas shows a PaO2 of 70 mm Hg on 100% FiO2. Bedside echocardiography confirms normal left ventricular (LV) systolic function. A nasopharyngeal swab tests positive for influenza A.
Clinical Case Scenario 2
A 75-year-old man with diabetes mellitus, hypertension, and peripheral vascular disease underwent infra-renal endovascular repair (EVAR) of an 8-cm abdominal aortic aneurysm. Administration of iodinated contrast was used during the procedure. On day 3 following the procedure, serum creatinine rose from a preoperative value of 112 µmol/L to 150 µmol/L. Doppler ultrasound of renal vessels showed no abnormality. Bedside volume assessment using ultrasound was suggestive of euvolemia. A diagnosis of contrast-induced nephropathy (CIN) was suggested.
Clinical Case Scenario 1
An elderly woman, aged 76 and weighing 75 kg, is hospitalized to the Intensive Care Unit (ICU) with urosepsis. She experiences stage 3 Acute Kidney Injury (AKI). The urine output is 15-30 millilitres per hour. The creatinine level is 3.6 milligrams per deciliter (318.3 micromoles per litre). The urea level is 26 millimoles per litre. The potassium level is 5.2. The base excess is -7. Her current dosage of Noradrenaline support is 0.4 micrograms per kilogram per minute. The patient is currently on mechanical ventilation with a fraction of inspired oxygen (FiO2) of 0.6 and positive end-expiratory pressure (PEEP) of 10. The cumulative fluid balance is a positive 6 litres on the third day of the patient’s stay in the intensive care unit. Below are the important vital parameters. What is the optimal management strategy?
Clinical Case Scenario 2
Which antibiotic requires dose adjustment in a patient with creatinine clearance of 20 mL/minute/1.73 m2?